Key Insights
| According to data from the Notifiable Diseases in Nova Scotia 2022 Surveillance Report, the province recorded a total of 27 HIV cases, which is a rate of 2.6 individuals per 100,000 population. The same report shows that during the same year, the HIV diagnosis rate for men was 4.6 per 100,000 population, while the rate for females was 0.8. Statistics Canada shows that in 2022, Canada had a total of 1,833 new cases of first-time HIV diagnosis, which is a rate of 4.7 individuals per 100,000 population. Data from Statista reveals that in 2022, Halifax had an HIV incidence rate that was lower than most areas in the country. This rate is 86.3% lower than the highest spot, Saskatchewan, at 19 cases. The Institute of Health Economics illustrates that the lifetime cost for one HIV diagnosis is $1,438,169 per individual. |
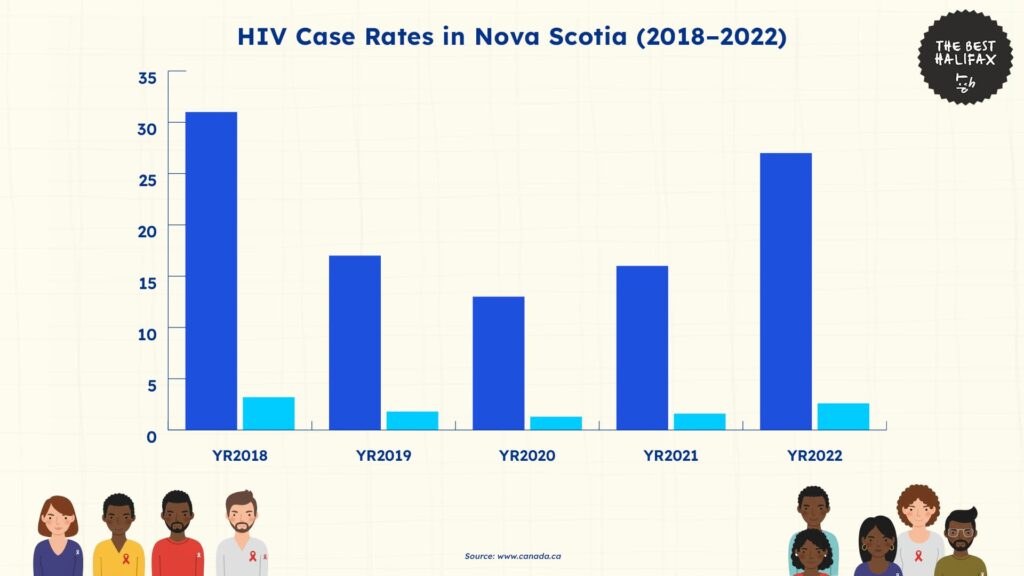
The Notifiable Diseases in Nova Scotia 2022 Surveillance Report reveals that Nova Scotia had 27 confirmed human immunodeficiency virus (HIV) cases in 2022, with a corresponding rate of 2.6 individuals per 100,000 population.
This is the highest number and rate of HIV cases in the province since 2018, which highlights a growing cause for concern.
The 2022 value is also a 68.8% increase in the number of cases from the 16 reported in 2021 and a 62.5% increase from the rate of 1.6 individuals per 100,000 population.
Moreover, this rate has been increasing since 2021 after a consistent trend of decreasing case numbers during previous years.
Between 2018 and 2020, Nova Scotia experienced a consistent decline in HIV diagnoses. Case numbers dropped by 58.1% from 31 in 2018 to 13 in 2020.
Over the same period, the rate per 100,000 fell from 3.2 to 1.3, which is a 59.4% decrease. While these numbers may be attributed to a lower rate of HIV transmission, it is important to note that this may have also been affected by the COVID-19 pandemic.
For example, changes in public behavior due to quarantine, limited testing access during the pandemic, or interruptions in surveillance and care systems may have all affected these lower rates.
Nevertheless, the upward trend started in 2021, when the number of cases increased from 13 to 16.
The two-year rise from 2020 to 2022 is 107.7% in raw cases and 100% in rate. This is a close return to the levels seen in 2018 but has not yet surpassed the last peak of 31 cases.
National HIV Trends in Canada
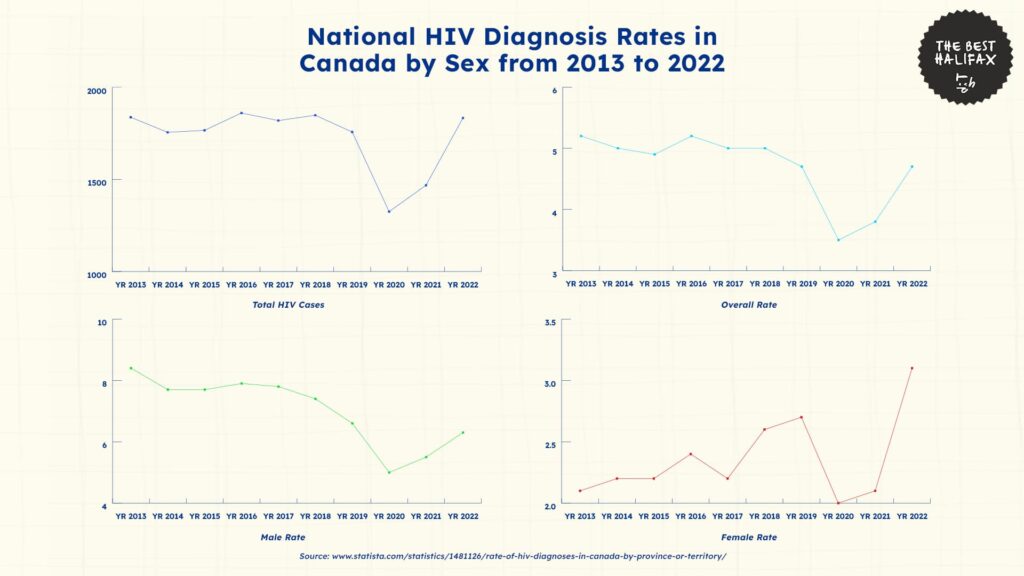
Statistics Canada shows that Canada had 1,833 new cases of first-time HIV diagnosis in 2022, which is a rate of 4.7 individuals per 100,000 population.
This illustrates a rise in case counts of 24.9% compared to 2021, when 1,468 diagnoses were registered. Meanwhile, the total rate also had a rise of 14.6% at 4.1 individuals.
The rise in both overall diagnoses and rate is a contrast to the drop seen in 2020 when the nationwide total dipped to 1,325 cases and the rate decreased to 3.5.
However, there is also a need to consider changes in national surveillance methods. The Public Health Agency of Canada notes that they changed their reporting thresholds in 2020 to only first diagnoses of HIV.
While this led to a noticeable drop in reported cases that year, this did not directly mean fewer transmissions were occurring.
Meanwhile, the steady rise in the following years also indicates a return to pre-pandemic trends, which could also possibly be due to revived testing, shifts in personal health behavior, and enhanced reporting of cases.
The data also reveals persistent sex-based differences in total HIV transmission incidences.
In 2022, the male rate was 6.3 per 100,000, which is almost two times higher than the rate for females at 3.1.
Furthermore, while both rates have fluctuated since 2013, the rate for males continues to be consistently higher.
Notably, though, from 2013 to 2019, the male rate fell from 8.4 to 6.6. Meanwhile, the female rate modestly increased from 2.1 to 2.7.
Regional Analysis of HIV Trends Across Canada
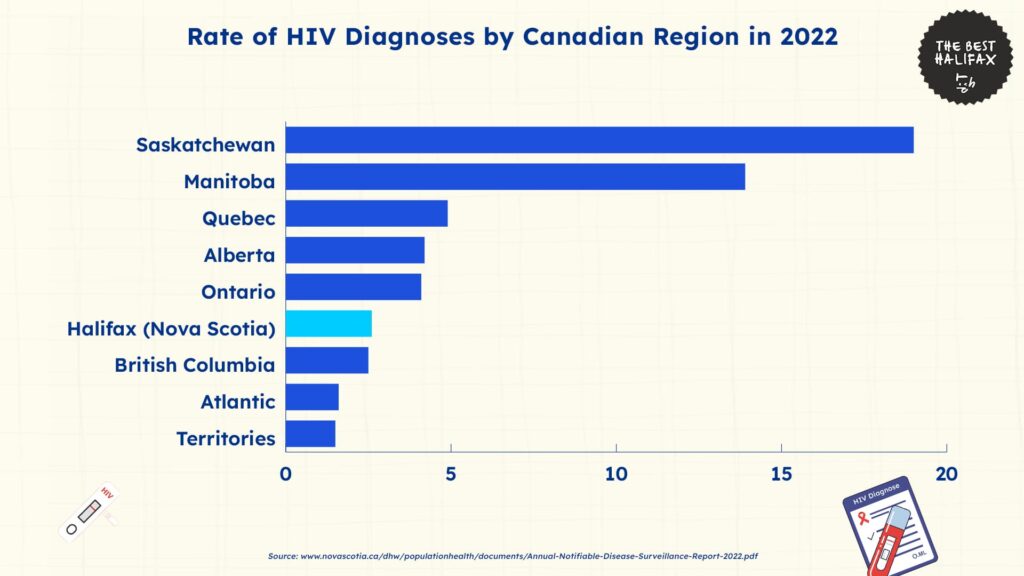
Data from Statista reveals insights into the trend of HIV cases across Canada in comparison to that of Halifax in 2022.
In 2022, Halifax had an HIV diagnosis rate of 2.6 per 100,000 population. This is much lower than the rate for many other Canadian areas.
Out of the eight largest jurisdictions monitored, Halifax is in sixth place, ahead of British Columbia, the Atlantic regions, and other territories.
The highest rate in the country is from Saskatchewan, with 19 recorded cases. This rate is over seven times higher than in Halifax, which could be an indicator of the high public health burden in the province.
Manitoba recorded the second-highest number of 13.9 cases, which is 434.6% higher than Halifax’s rate. This shows how both of the top two provinces are disproportionately affected by new HIV diagnoses, indicating the growth of ongoing transmission patterns.
In central Canada, Quebec had a rate of 4.9 or 88.5% above that of Halifax. Meanwhile, Alberta and Ontario had slightly lower rates at 4.2 and 4.1, which are still 61.5% and 57.7% above that of Halifax, respectively.
While these provinces are in the mid-range provincially, they still have significantly higher rates of HIV diagnoses than Halifax.
British Columbia had a rate of 2.5, which is slightly lower than Halifax’s 2.6. This puts both areas in roughly the same range, indicating that these provinces have stronger health infrastructures than others.
Meanwhile, Halifax’s rate of HIV transmission was 62.5% greater than the regional average in Atlantic of 1.6. Similarly, the Territories had a rate of 1.5, which is 42.3% lower than Halifax.
Overall, the rate of first-time HIV transmissions in Halifax is much lower when compared to other areas in the country, which indicates that they have stronger interventions against HIV.
Demographic Breakdown of HIV Trends in Nova Scotia
Data from the Notifiable Diseases in Nova Scotia 2022 Surveillance Report shows how HIV disproportionately affects different populations in the province.
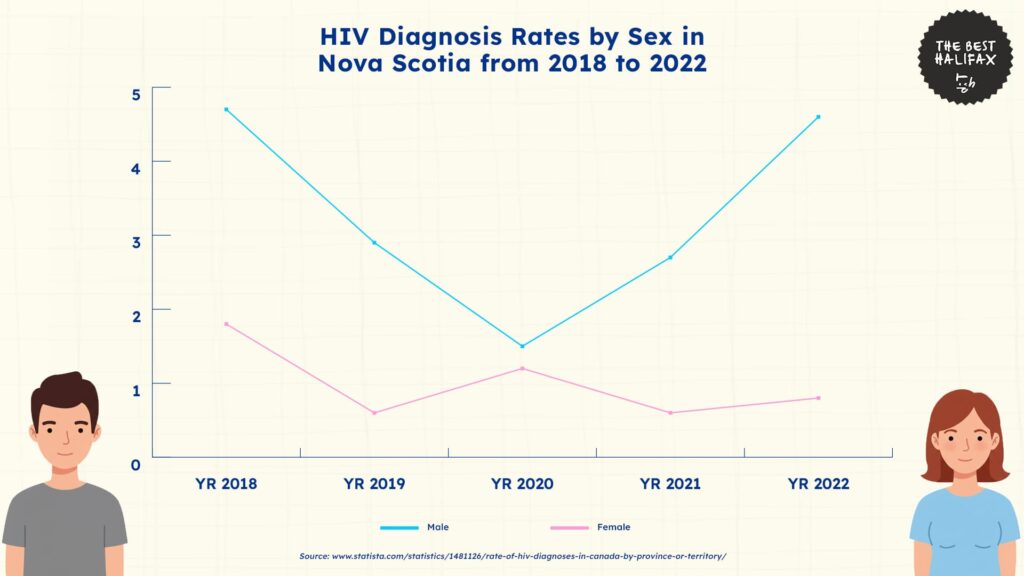
HIV Trends by Gender
In 2022, the rate of HIV diagnosis for men in Nova Scotia was 4.6 per 100,000 population, and for females, it was 0.8.
This puts the male rate at 475% higher than the female rate. This gender gap in 2022 is also the largest across the five years from 2018 to 2022.
Moreover, a large portion of the total rise in provincial HIV cases comes from the rise in the rate for males, as they had the highest increases in rates for this period.
Between 2018 and 2020, the rate for males did drop by 68.1%, decreasing from 4.7 to 1.5.
However, beginning in 2020, the male rate increased each subsequent year, from 1.5 in 2020 to 2.7 in 2021 and again to 4.6 in 2022.
During the period from 2020 to 2022, the HIV rate among males increased by 206.7% in only two years. This increase brings the male rate close to where it was in 2018, at 4.7.
Conversely, the rate of female HIV diagnoses has been consistently low and fairly constant.
Their number of cases dropped from 1.8 in 2018 to 0.6 in both 2019 and 2021, while also decreasing temporarily to 1.2 in 2020.
In 2022, the figure went up, but only very slightly, to 0.8. This is 55.6% lower than the rate in 2018, which indicates a steady decline in cases for females.
Overall, the data shows a large disparity in HIV cases by gender. This points to a need for gender-specific interventions in Halifax, given that men in the city are much more vulnerable to HIV transmission.
HIV Trends by Age
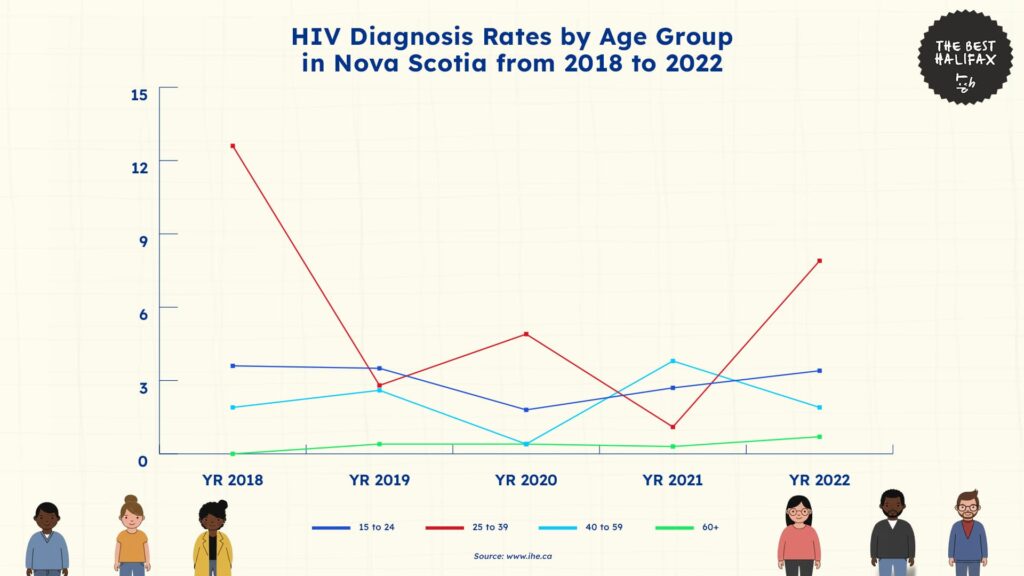
Between 2018 and 2022, HIV diagnosis rates in Nova Scotia varied greatly across age groups, with notable trends between young and old populations.
Children aged 0 to 4 and children aged 5 to 14 always reported a rate of 0 per 100,000 population for all five years. This shows that there were no confirmed HIV diagnoses among people under the age of 15 during this time.
The total lack of reported cases in these age groups indicates a very low transmission risk in early childhood and pre-adolescence.
In the 15 to 24 years age group, the rate varied from year to year. It started at 3.6 in 2018 and remained fairly consistent in 2019 at 3.5.
This rate fell to 1.8 in 2020 before rising again to 2.7 in 2021 and 3.4 in 2022. Though these numbers fluctuated, this group consistently had one of the highest rates every year, reflecting continued HIV exposure or detection in young adults.
For the age group 25 to 39, HIV diagnosis rates were often the highest across age groups each year, except for 2019 and 2021.
The rate was highest at 12.6 in 2018, then fell to 2.8 in 2019, and increased again to 4.9 in 2020. Even though it fell to 1.1 in 2021, the rate then jumped significantly to 7.9 in 2022, showing that this group also had the highest volatility.
In the 40 to 59 age group, rates were steadier. The highest rate was 3.8 in 2021, then it dropped to 1.9 in 2022. While not the leading age group impacted, this group still contributes a significant share of cases yearly.
Among those aged 60 and above, HIV rates of diagnosis were low for all years. The rates for this group increased from 0 in 2018 to 0.4 in 2019 and 2020, decreased to 0.3 in 2021, and slightly increased to 0.7 in 2022.
Although small in number, these cases prove that older individuals are not free from the risks of HIV and should remain a factor in healthcare planning.
In summary, the statistics highlight that HIV in Nova Scotia is highest among adults between 15 and 39 years.
The two groups here had overall rates of 3 and 5.86, respectively, which are higher than any other group.
These results highlight the importance of targeted prevention and education programs for adolescents, young adults, and early middle-aged groups.
Costs and Consequences of Rising Cases of HIV in Canada
Long-Term Financial Burden Per Case of HIV
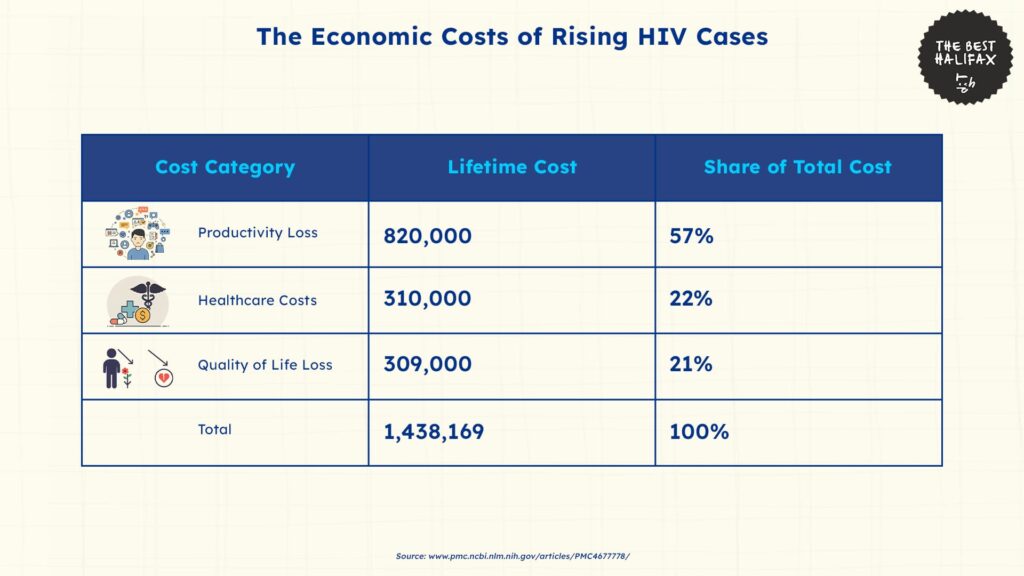
The Institute of Health Economics found that the lifetime expense of caring for one HIV diagnosis in Canada has increased dramatically, now standing at $1,438,169.
This represents an 11% increase over earlier estimates and captures the economic burden of supporting lifelong treatment, support services, and the indirect effects of living with the disease.
Moreover, this estimate encompasses regular antiretroviral therapy, laboratory monitoring, specialist consultations, hospitalization, and loss of employment and quality of life.
In contrast, previous estimates in 1997 by the Health Network set the lifetime cost at $153,000 per individual.
The dramatic rise between previous and recent projections shows how the spread and the chronic nature of HIV have rendered the disease progressively more expensive to treat over the long term.
This updated cost of $1.44 million per individual is divided into three major components.
Productivity losses account for 57% of this cost, or $820,000 per person, and represent the largest share. These losses stem from reduced ability to work due to illness, time off for treatment, early retirement, and in some cases, premature death.
The economic impact is felt both at the individual level through reduced earnings and at the national level through lower overall labor market participation.
Healthcare costs make up 22%, amounting to $310,000 per person. This includes long-term medication, outpatient and inpatient care, laboratory testing, and support services.
Although HIV treatment has become more effective, it remains resource-intensive and must continue uninterrupted throughout a person’s life to maintain viral suppression and prevent transmission.
Meanwhile, quality of life losses contribute the remaining 21%, or $309,000 per person. This category accounts for reductions in mental health challenges and limitations in daily activities.
While not always directly measured in dollars, these effects have real economic value through reduced life satisfaction and greater dependence on support systems.
National Costs and Impacts of Rising HIV Cases
The lifetime cost burden of new HIV diagnoses adds up over time. As per the existing per-case estimate, the 1,468 new cases registered in 2021 meant an estimated $2.1 billion in lifetime economic expenses.
In 2022, this number increased to $4.7 billion, and in 2023, it was $8.2 billion, at constant or rising levels. These numbers do not include short-term spending, but instead the overall future costs of those who were diagnosed each year.
As a result of increased per-case lifetime costs and rising incidences, the actual total is estimated to be much higher.
These escalating numbers highlight the long-term economic consequence of each new diagnosis and persistent pressure on health systems, social services, and labor markets.
Moreover, the Health Network reported that HIV cases have often affected more vulnerable populations, such as injection drug users, LGBTQ+ individuals, aboriginal populations, and at-risk women.
These groups frequently experience barriers to proper healthcare, secure housing, and employment, which increases not only transmission risk but also the cost of care and support.
Interventions and Solutions to Rising HIV Cases
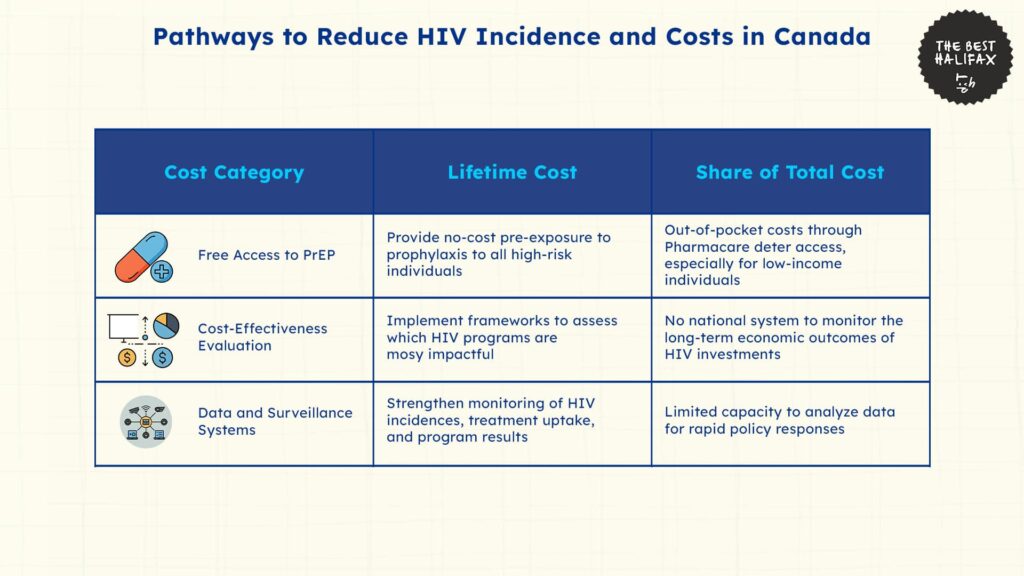
Canada’s growing HIV epidemic has led to new demands for prevention efforts and more equitable treatment distribution.
Recent analysis has shown two priority focus areas in the enhancement of access to preventive medication options and better cost-effective frameworks of investment.
One of the most successful methods of preventing new HIV infections is access to pre-exposure prophylaxis (PrEP). PrEP is a highly effective drug that, when taken regularly, can lower the risk of contracting HIV by over 90%.
However, in areas across Canada like Halifax, access is still unequal. CBC News reports that while the province of Nova Scotia covers PrEP under its Pharmacare program, many people are still required to pay deductibles and co-payments.
These out-of-pocket expenses are still a significant barrier, particularly for low-income and vulnerable populations.
Nova Scotia health advocates and opposition parties have demanded that PrEP be provided free of cost to everyone who requires it. This is justified by public health data that shows that Nova Scotia reported the highest rate of HIV in five years in 2022.
If broader access to preventive care does not increase, the province can expect continued increasing incidences of HIV cases.
Moreover, supporters stress that access to PrEP on an economic level is not only a health concern but an issue of fairness.
Individuals in at-risk groups, like the youth, racial minorities, and LGBTQ+ individuals, tend to experience financial as well as social constraints to regular prevention.
Eliminating all cost barriers would most likely drive up usage and enable Nova Scotia to prevent the rise of more HIV cases.
In addition to individual interventions, Canada also needs to fill gaps in how it monitors and manages the economic effectiveness of its HIV response.
The Institute of Health Economics (IHE) reports that the lifetime cost of a single HIV diagnosis is now over $1.4 million, and most of that burden is tied to productivity loss and quality-of-life effects rather than healthcare costs.
The IHE has identified a key flaw in the nation’s response to HIV, in that there is no national framework for evaluating the cost-effectiveness of Canada’s HIV-related investments.
Canada invested around $687 million in HIV-related programs in 2017. However, due to a lack of tracking and evaluation, it cannot be determined which interventions offered the greatest value for money.
This lack of performance monitoring slows down the creation of successful models or redirects funding away from less effective methods.
Moreover, the IHE points out that prevention, especially when addressed at high-risk groups, has some of the best returns on investment.
However, this needs initial planning, consistent financing, and systems for tracking long-term results. Improved surveillance tools, enhanced data infrastructure, and standardized evaluation systems are needed to align spending with effect.
The Future of HIV Trends in Halifax
According to current HIV incidence and cost trends, the economic placed on Halifax will only continue to rise unless strong interventions are made.
As treatment extends life expectancy, the cumulative cost of managing HIV will only grow.
Unless there is increased access to prevention services and more effective national strategies, new cases will likely remain at present levels or steadily climb.
Even a small increase in yearly diagnoses would produce higher costs that strain public resources even further. In places like Halifax, where rates have already increased substantially in recent years, this situation is even more alarming.
On the other hand, even modest decreases in new diagnoses would create significant long-term savings.
Reducing incidences through no-cost PrEP programs, focused outreach, and low-cost interventions would decrease the overall financial burden for both healthcare systems and the productivity and quality of life of individuals.
Ultimately, the projections are in two directions: a high-cost trajectory characterized by increasing or stable incidence, or a more sustainable path conditioned by initial, concerted action. The coming years will decide which one becomes Canada’s reality.
References
- Nova Scotia Department of Health and Wellness. (2023). Annual notifiable disease surveillance report 2022. https://novascotia.ca/dhw/populationhealth/documents/Annual-Notifiable-Disease-Surveillance-Report-2022.pdf
- Statista. (2023). Rate of HIV diagnoses in Canada in 2022, by province or territory. https://www.statista.com/statistics/1481126/rate-of-hiv-diagnoses-in-canada-by-province-or-territory/
- Public Health Agency of Canada. (2023). HIV in Canada: Surveillance report to December 31, 2022. Government of Canada. https://www.canada.ca/en/public-health/services/publications/diseases-conditions/hiv-canada-surveillance-report-december-31-2022.html#a10.1
- Institute of Health Economics. (2023). Lifetime cost of HIV in Canada now exceeds $1.4 million. https://www.ihe.ca/news/updates/lifetime-cost-hiv#:~:text=Economic%20Cost%20of%20HIV%20in,compared%20to%20a%20decade%20ago.
- Krentz, H. B., & Gill, M. J. (2015). The direct medical costs of late presentation (<350/mm³) of HIV infection over a 15-year period. AIDS Research and Treatment, 2015, Article 236043. https://pmc.ncbi.nlm.nih.gov/articles/PMC4677778/
- Canadian Policy Research Networks. (2003). Assessing the economic burden of HIV/AIDS in Canada. https://oaresource.library.carleton.ca/cprn/18424_en.pdf
- CBC News. (2023, November 30). HIV cases in Nova Scotia hit highest point in 5 years as advocates call for free prevention drug. https://www.cbc.ca/news/canada/nova-scotia/hiv-cases-rise-opposition-parties-advocates-no-cost-access-prevention-meds-1.7365203
- Nova Scotia Department of Health and Wellness. (2023). HIV/AIDS surveillance report. https://novascotia.ca/DHW/POpulationhealth/documents/HIV-AIDS-Surveillance-Report.pdf